Halloween decorations and supplies are lining store shelves and fall weather and colors will (hopefully) arrive soon, but a more important season is already here and it doesn’t come with the same fanfare — open enrollment season! That’s right, it’s time to review, adjust, and enroll in your employee benefits plans for the coming year. From September through November, open enrollment gives employees a short window to sign up, update, or cancel health insurance and voluntary benefit plans. With health costs rising, voluntary benefits expanding, and digital enrollment tools becoming the norm, 2026 presents new opportunities—and challenges—for both employers and employees.
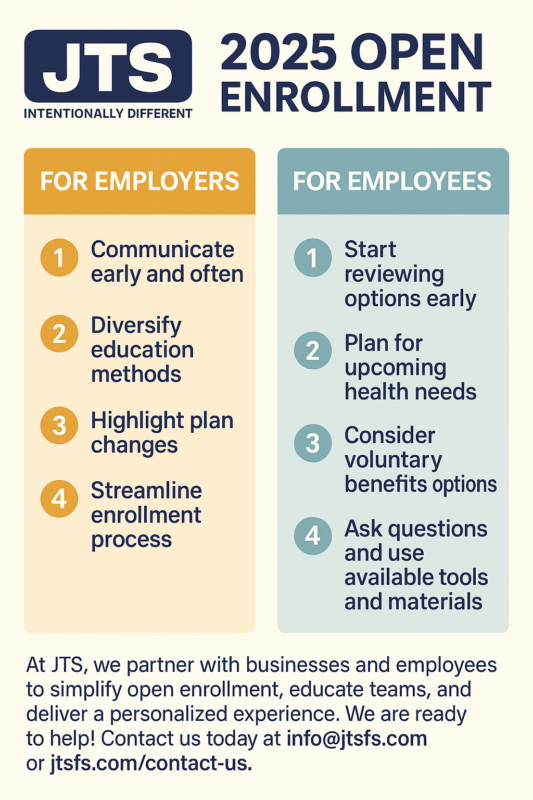
To make the most of this year’s open enrollment, here’s a basic breakdown of some best practices and advice for employers and employees:
For Employers & HR Teams
- Start Early and Plan Deliberately
- Begin communicating 8–12 weeks in advance.
- Audit existing benefits, vendor contracts, and employee usage trends before enrollment.
- Use Multi-Channel, Bite-Sized Communication
- Go beyond email: webinars, short videos, infographics, and text reminders resonate more.
- Always highlight: What’s new / What’s changing / What stays the same.
- Simplify the Decision Process
- Provide side-by-side comparisons of premiums, deductibles, and networks.
- Spotlight Underutilized and Voluntary Benefits
- Reintroduce lesser-known benefits like commuter perks, tuition reimbursement, or wellness programs.
- Add trending voluntary benefits: accident, critical illness, hospital indemnity, student loan assistance, or legal aid.
- Show cost vs. value clearly to overcome hesitation.
- Leverage Data and Feedback
- Track enrollment patterns, portal usage, and help desk volume in real time.
- Run post-enrollment surveys to refine next year’s strategy.
- Train Internal Champions
- Ensure managers and HR liaisons have critical information (or “cheat sheets”) for answering questions.
- Host “office hours” or Q&A sessions.
- Frame Benefits as Financial Security
- Position benefits as a safety net during uncertain economic times.
- Be transparent about cost increases and regulatory changes.
- Keep Engagement Going Post-Enrollment
- Send quarterly “benefits refreshers.”
- Offer ongoing support through a benefits help desk or concierge.
For Employees
- Don’t Default—Review Annually
- Your health needs and costs change. Don’t simply auto-renew last year’s elections.
- Start Early
- Review options before the deadline rush to avoid last-minute stress.
- Project Healthcare Usage
- Look at last year’s expenses, medications, and anticipate changes like new treatments or surgeries.
- Understand Total Cost of Coverage
- Compare premiums, deductibles, copays, and out-of-pocket maximums—not just monthly premiums.
- Maximize Tax-Advantaged Accounts
- HSAs and FSAs can save you money on healthcare and dependent care costs.
- Evaluate Voluntary Benefits
- Supplemental coverage can protect against high out-of-pocket costs if you face an accident or illness.
- Ask Questions
- If something is unclear, reach out to HR or your benefits specialist.
- Use the Tools Available
- Decision support platforms, benefit calculators, and live Q&A sessions are there to help you.
- Save Your Documentation
- Keep plan summaries and enrollment confirmations for quick reference.
- Remember Mid-Year Flexibility
- Know your options if you have a qualifying life event (marriage, birth, loss of coverage).
Closing Thoughts
Open enrollment doesn’t have to be stressful. With the right preparation, communication, and tools, employers can boost engagement while employees make smarter choices.
At JTS, we partner with businesses and employees to simplify open enrollment, educate teams, and deliver a personalized experience across multiple channels. Go into open enrollment confident and informed—contact us today to learn more.